The urinary system is often described as a simple drainage network. It filters blood, produces urine, and eliminates waste. But beneath that simplicity lies a remarkably sophisticated defense system.
Every day, the urinary tract encounters bacteria from the skin, digestive tract, and surrounding environment. Despite this constant exposure, most people do not develop a UTI every day. That is because the urinary tract is not passive. It is biologically prepared to defend itself.
Understanding how the body protects against uti infection helps explain why some individuals develop recurrent infections while others do not. It also clarifies how factors like bladder irritation, hormonal changes, or weakened immunity can disrupt this delicate balance.
This article explores the immune mechanisms of the urinary tract, how infections develop, and why utis in women are particularly common.
Overview of the Urinary System
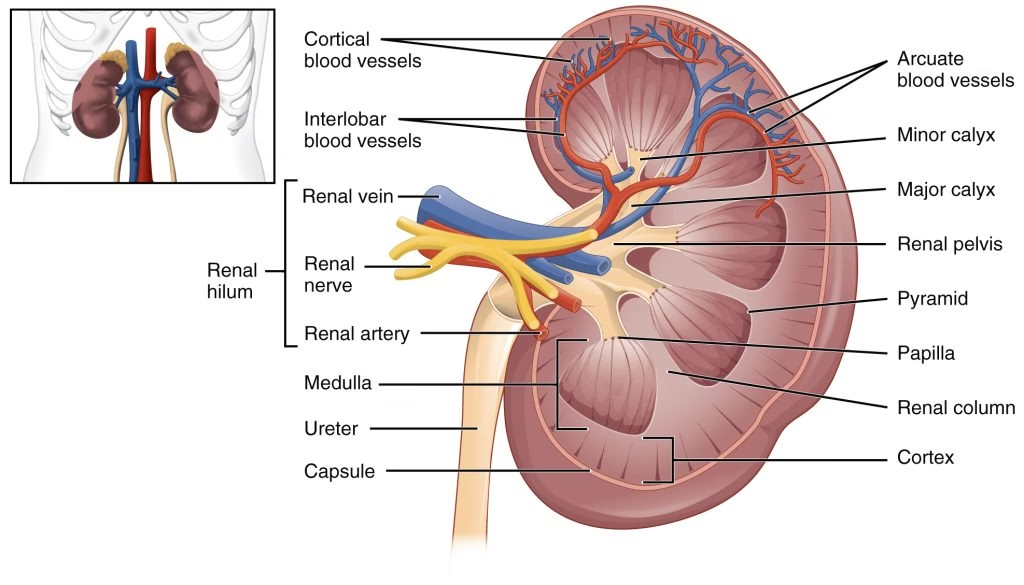
The urinary tract consists of:
- Kidneys
- Ureters
- Urinary bladder
- Urethra
Each component plays a role in maintaining sterility.
- Kidneys filter blood and produce urine
- Ureters transport urine to the bladder
- The urinary bladder stores urine
- The urethra expels urine from the body
Despite being connected to the external environment, the upper urinary tract is normally sterile. This sterility is preserved through layered immune defenses.
How a UTI Infection Begins
A uti infection usually starts when bacteria enter the urethra and travel upward. The most common source is bacteria from the gastrointestinal tract.
The infection may remain localized in the bladder, known as a urinary bladder infection, or ascend further toward the kidneys.
Common types include:
- Lower urinary tract infection
- Bacterial infection in urine confined to the bladder
- Ureter infection
- Kidney infection
The severity depends on how far bacteria travel and how effectively the immune system responds.
Mechanical Defenses of the Urinary Tract
The first line of defense is mechanical rather than cellular.
Urine Flow
Regular urination physically flushes bacteria out of the urinary tract.
- Continuous urine flow prevents bacterial attachment
- Frequent voiding reduces bacterial colonization
When urine flow is obstructed, bacteria have more time to adhere to the lining.
Complete Bladder Emptying
Incomplete emptying allows bacteria to multiply in residual urine.
Conditions that impair bladder contraction increase infection risk.
Ureteral Valves
The ureters contain mechanisms that prevent backward flow of urine. This prevents bacteria from moving upward toward the kidneys.
Mechanical defenses are simple but highly effective under normal conditions.
The Protective Role of the Urothelium
The inner lining of the urinary tract is called the urothelium. It is not merely a surface. It functions as an active immune barrier.
The urothelium provides protection through:
- Tight cell junctions that block bacterial penetration
- Production of antimicrobial peptides
- Rapid cell turnover when infected
When bacteria attempt to attach, the urothelial cells can shed infected layers, physically removing bacteria.
This shedding mechanism is one reason mild infections may resolve quickly.
Chemical and Antimicrobial Defenses
The urinary tract also deploys chemical defenses.
Antimicrobial Peptides
Cells lining the urinary tract release small proteins that:
- Disrupt bacterial cell walls
- Inhibit bacterial growth
- Prevent colonization
Urine Composition
Urine itself contains factors that limit bacterial survival:
- Slight acidity
- High urea concentration
- Variable osmolarity
These conditions are not ideal for bacterial growth.
However, when urine becomes stagnant or diluted excessively, protective effects may weaken.
Immune Cells in the Urinary Tract
When bacteria overcome mechanical and chemical defenses, immune cells are activated.
Innate Immune Response
The innate immune system responds quickly.
- Neutrophils migrate to the infection site
- Macrophages engulf bacteria
- Inflammatory signals increase blood flow
This rapid response often produces symptoms such as:
- Burning during urination
- Frequent urge to urinate
- Bladder irritation
These symptoms reflect immune activation rather than just bacterial presence.
Inflammatory Response and Symptoms
Bladder irritation during a uti infection occurs because immune cells release signaling molecules.
These signals cause:
- Swelling of the bladder lining
- Increased sensitivity
- Urgency
- Pain
The discomfort is part of the body’s attempt to eliminate infection.
While unpleasant, inflammation is a sign that immune defenses are working.
Adaptive Immune Response
If bacteria persist, the adaptive immune system becomes involved.
This includes:
- Production of antibodies
- Activation of specific immune cells targeting the bacteria
However, immunity to UTI is often incomplete. Reinfections can occur, particularly if bacterial strains vary.
This explains why some individuals experience recurrent urinary bladder infection episodes.
Why UTIs in Women Are More Common
Anatomy plays a significant role in utis in women.
- The female urethra is shorter
- It is located closer to the anus
- Bacteria can travel upward more easily
Hormonal changes also influence susceptibility.
Lower estrogen levels can:
- Alter vaginal flora
- Reduce protective bacteria
- Increase infection risk
This combination of anatomical and hormonal factors explains the higher incidence.
Role of the Microbiome
The urinary tract was once believed to be completely sterile. Research now suggests a complex urinary microbiome exists.
Beneficial microbes may:
- Compete with harmful bacteria
- Reduce colonization
- Support immune signaling
Disruption of normal flora, such as after antibiotic use, can increase susceptibility to uti infection.
Balancing treatment with microbiome preservation is an evolving area of research.
Bacterial Strategies to Evade Immunity
Some bacteria are particularly effective at surviving immune attack.
They may:
- Form protective biofilms
- Hide within bladder cells
- Resist antimicrobial peptides
Biofilms create protective layers that shield bacteria from immune cells and even antibiotics.
This is one reason some infections recur despite treatment.
Risk Factors That Weaken Urinary Defenses
Several conditions impair natural defenses:
- Incomplete bladder emptying
- Dehydration
- Diabetes
- Hormonal changes
- Prolonged catheter use
- Immune suppression
When defenses weaken, bacteria gain advantage.
Chronic bladder irritation can also damage protective barriers.
Ureter Infection and Ascending Spread
If bacteria ascend beyond the bladder, they may cause ureter infection or kidney infection.
The body attempts to prevent this through:
- Ureteral peristalsis
- Immune cell activation
- Increased urine production
If these mechanisms fail, infection can spread and become more serious.
Early treatment reduces risk of progression.
UTI Treatment and Immune Recovery
Uti treatment typically involves antibiotics to eliminate bacteria.
However, antibiotics do not replace immune defenses. Instead, they reduce bacterial burden, allowing the immune system to regain control.
Supporting recovery involves:
- Adequate hydration
- Completing prescribed treatment
- Avoiding unnecessary antibiotic overuse
Repeated antibiotic use may disrupt protective flora, increasing vulnerability.
Balanced management is essential.
Prevention Strategies Based on Immune Principles
Understanding immune mechanisms helps guide prevention.
Effective strategies include:
- Staying hydrated
- Urinating regularly
- Maintaining hygiene
- Managing blood sugar levels
- Avoiding prolonged urinary retention
- Supporting vaginal flora balance
These actions reinforce natural defense layers.
When to Seek Medical Care
Seek evaluation if you experience:
- Burning urination
- Frequent urination
- Cloudy urine
- Fever
- Lower back pain
- Persistent bacterial infection in urine
Prompt treatment prevents spread to the upper urinary tract.
Recurring infections require deeper evaluation to identify underlying causes.
Final Thoughts
The urinary tract is not defenseless. It is protected by mechanical flushing, cellular barriers, antimicrobial compounds, immune cells, and microbiome balance.
A uti infection develops only when bacteria overcome multiple layers of protection.
From urinary bladder infection to ureter infection, the progression depends on how effectively these defenses respond.
Understanding immune mechanisms clarifies why utis in women are more common and why some individuals experience recurrent episodes.
Supporting urinary health means strengthening these natural defenses through hydration, hygiene, balanced treatment, and timely medical care.
The body is designed to protect itself. When infections occur, they are signals that defenses need support.