Celiac disease is a chronic autoimmune condition that affects millions of people worldwide, yet it is still widely misunderstood and often misdiagnosed. Many people live for years without realizing that their persistent digestive discomfort, nutritional deficiencies, or unexplained fatigue are connected to gluten consumption. Understanding celiac disease meaning, its causes, symptoms, diagnostic process, treatment options, and prevention strategies is essential for long-term health.
This comprehensive guide outlines everything you need to know about celiac disease, including the pathology, testing methods, diet guidelines, and specific signs such as celiac disease symptoms in females, who are statistically more likely to be diagnosed.
What Is Celiac Disease?
Celiac disease is an autoimmune disorder where the immune system reacts abnormally to gluten, a protein found in wheat, barley, and rye. When someone with celiac disease consumes gluten, the immune response damages the small intestine’s villi — small, finger-like structures responsible for absorbing nutrients. Over time, this damage leads to malnutrition, digestive issues, and widespread systemic problems.
Celiac Disease Meaning (Simplified)
A long-term immune reaction to gluten that injures the small intestine and causes nutrient absorption problems.
Unlike gluten intolerance or wheat allergy, celiac disease is a lifelong condition that requires strict dietary adherence and medical supervision.
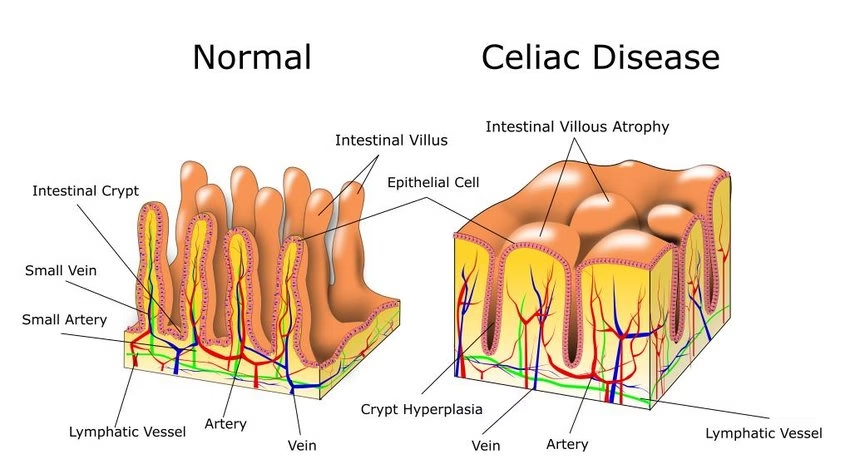
Celiac Disease Pathology Outlines
Understanding the pathology helps clarify why symptoms vary so much. In celiac disease:
- The immune system attacks the intestinal lining when gluten is consumed.
- Villi atrophy (flatten), reducing nutrient absorption.
- Chronic inflammation develops in the small intestine.
- Malabsorption leads to deficiencies in iron, calcium, folate, vitamin D, and other nutrients.
Pathology reports often show:
- Villous atrophy
- Crypt hyperplasia
- Increased intraepithelial lymphocytes
These changes form the basis for diagnosis when biopsies are taken.
Common Celiac Disease Symptoms
Symptoms can vary widely from person to person. Some experience severe digestive issues, while others show no gastrointestinal symptoms at all. Children, adults, and females may present differently.
Digestive Symptoms
- Chronic diarrhea
- Constipation
- Bloating and gas
- Abdominal pain
- Fatty stools
- Nausea or vomiting
Non-Digestive Symptoms
- Unexplained weight loss
- Fatigue and low energy
- Iron deficiency anemia
- Joint pain
- Headaches or migraines
- Osteopenia or osteoporosis
- Tingling or numbness in hands and feet
- Skin rash (dermatitis herpetiformis)
- Mouth ulcers
Celiac Disease Symptoms in Females
Women may experience additional signs, including:
- Irregular periods
- Fertility issues
- Miscarriage risk
- Early menopause
- Hair loss
- Severe anemia
- Bone pain from calcium deficiencies
Because these symptoms overlap with thyroid disorders, PCOS, and hormonal imbalances, many women receive delayed or incorrect diagnoses.
What Causes Celiac Disease?
The exact cause is unknown, but several factors contribute to its development.
-
Genetic Predisposition
Most individuals with celiac disease have HLA-DQ2 or HLA-DQ8 genes.
Having these genes does not guarantee development but increases susceptibility.
-
Immune System Response
The immune system mistakenly identifies gluten as harmful, triggering inflammation.
-
Environmental Triggers
Certain factors can activate or worsen celiac disease:
- Viral infections
- Early childhood gluten exposure
- Gut microbiome imbalances
- Stress or major life changes
-
Family History
First-degree relatives have a higher risk.
Risk Factors for Celiac Disease
You are more likely to develop celiac disease if you:
- Have a relative with celiac disease
- Have autoimmune conditions (type 1 diabetes, thyroid disease)
- Are female
- Have Down syndrome or Turner syndrome
- Have microscopic colitis
- Have unexplained anemia or nutritional deficiencies
Celiac Disease Diagnosis
Diagnosing celiac disease can be complex. Symptoms may mimic other digestive disorders such as IBS, lactose intolerance, or Crohn’s disease. A step-by-step approach is used to confirm diagnosis.
-
Blood Tests (Celiac Disease Blood Test)
These tests look for specific antibodies that rise when gluten is consumed:
- tTG-IgA (tissue transglutaminase) – most common
- EMA-IgA (endomysial antibodies)
- DGP (deamidated gliadin peptides)
- Total IgA levels to rule out IgA deficiency
Blood tests should be done while the patient is still eating gluten regularly.
-
Genetic Tests
HLA-DQ2 and HLA-DQ8 gene testing helps rule out celiac disease in unclear cases.
-
Endoscopy and Biopsy
This is the gold standard for diagnosis. During an endoscopy:
- A thin tube is passed into the intestine
- Tissue samples are taken from the small intestine
- Pathology outlines villous atrophy and inflammation
-
Celiac Disease ICD-10 Code
The ICD-10 code for celiac disease is K90.0 — used for medical records, insurance, and documentation.
Celiac Disease Treatment
The only effective treatment is a strict, lifelong gluten-free diet.
-
Gluten-Free Diet
Eliminate all sources of:
- Wheat
- Barley
- Rye
- Cross-contaminated grains
Follow a structured celiac disease diet plan that includes whole foods like millet, rice, quinoa, vegetables, legumes, and gluten-free grains.
-
Nutritional Supplements
Deficiencies commonly require supplementation:
- Iron
- Folate
- Vitamin B12
- Calcium and vitamin D
- Zinc
-
Medications (as needed)
- Steroids may be prescribed for severe inflammation.
- Topical treatments help dermatitis herpetiformis.
-
Follow-Up Monitoring
Regular check-ups ensure healing and help track symptoms and antibody levels.
Prevention Strategies
While celiac disease cannot be fully prevented, the severity of symptoms can be minimized with early detection and a healthy lifestyle.
Key Prevention Approaches
- Recognize early symptoms and seek testing
- Follow a strict gluten-free diet if diagnosed
- Monitor nutrient levels
- Maintain gut health with fiber-rich, balanced meals
- Educate family members if there is a genetic risk
Living with Celiac Disease
With the right diet and medical support, individuals with celiac disease can live full, healthy lives. Early diagnosis, proper nutritional care, and lifestyle adjustments help prevent long-term complications such as osteoporosis, infertility, neurological issues, and growth problems.
Understanding celiac disease symptoms and recognizing how diverse they can be is the first step toward effective treatment and long-term wellness.