I still remember the first time I truly understood that trauma does not simply “go away.” For years, I believed that painful experiences fade with time. But as I learned more about post-traumatic stress disorder (PTSD), I realized that trauma can settle deep within the mind and body, shaping thoughts, emotions, and behavior long after the event has passed.
Post-traumatic stress disorder is more than a reaction to stress. It is a serious mental health condition that develops after experiencing or witnessing a traumatic event. It can affect anyone—children, adults, men, women, military veterans, accident survivors, or individuals who have endured abuse. Through my journey of learning about psychological health and observing how trauma impacts people differently, I’ve come to understand how crucial mental health awareness truly is.
In this article, I want to share what PTSD is, how it affects mental health and wellbeing, its symptoms, causes, diagnosis, treatment options, and practical steps toward recovery.
What Is Post-Traumatic Stress Disorder?
Post-traumatic stress disorder is a psychiatric condition triggered by experiencing or witnessing a traumatic event. These events may include:
- Physical or sexual assault
- Severe accidents
- Natural disasters
- War or combat exposure
- Domestic violence
- Childhood abuse or neglect
- Sudden loss of a loved one
Not everyone who experiences trauma develops PTSD. In fact, most people feel distress temporarily and gradually recover. However, when symptoms persist for more than a month and interfere with daily functioning, it may indicate PTSD.
What makes PTSD particularly challenging is how it disrupts mental stability. Trauma reshapes the way the brain responds to stress, danger, and memory. The body may remain in a constant state of alertness, even when no threat exists.
How Trauma Affects the Brain and Psychological Health
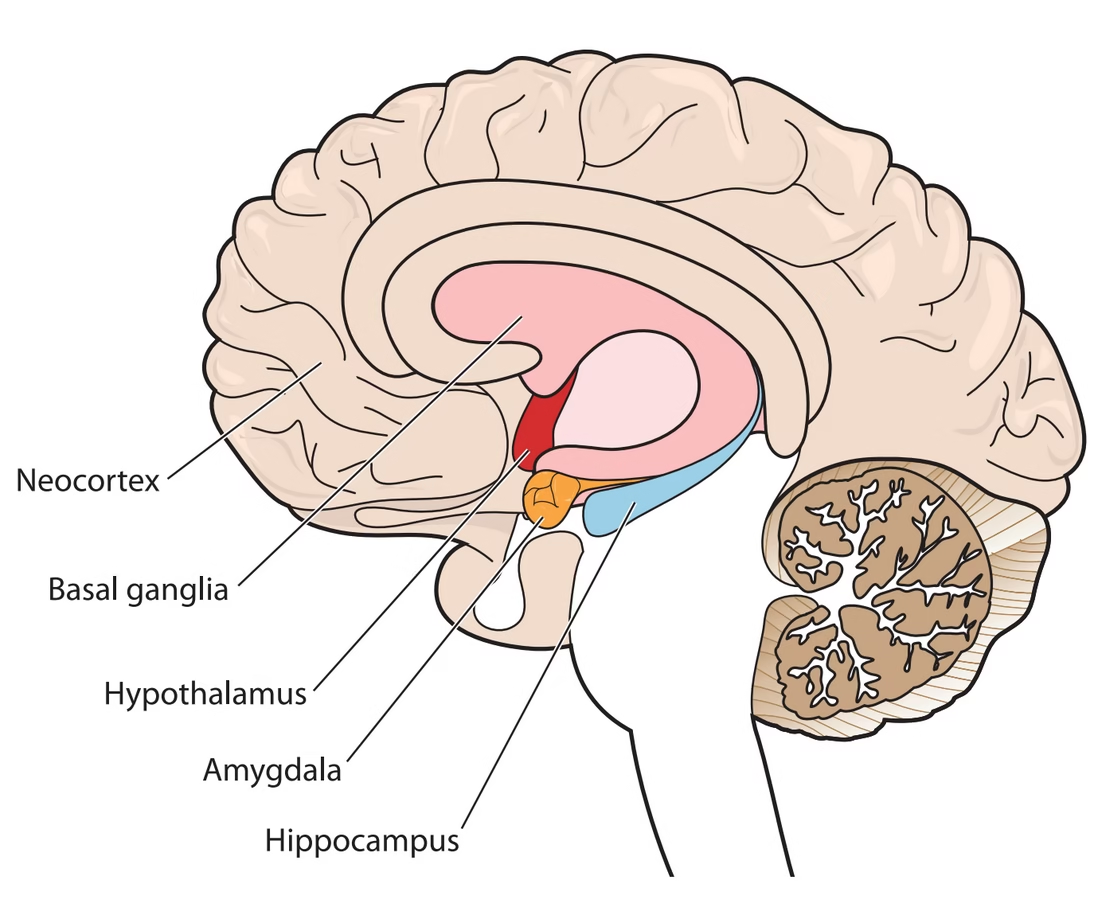
As I explored the science behind trauma, I discovered that PTSD is deeply connected to changes in brain function.
- The amygdala becomes overactive, increasing fear responses.
- The hippocampus, which processes memory, may shrink or function differently.
- The prefrontal cortex, responsible for decision-making and emotional regulation, may struggle to calm fear responses.
These changes explain why people with PTSD may:
- Relive traumatic memories repeatedly.
- Experience intense emotional reactions to reminders.
- Struggle with concentration or decision-making.
- Feel constantly on edge.
Understanding this biological component helped me shift from judgment to compassion. PTSD is not weakness. It is a mental health condition rooted in how the brain processes trauma.
Common Symptoms of PTSD
The symptoms of PTSD typically fall into four main categories.
-
Intrusive Symptoms
- Flashbacks that feel real and vivid
- Recurrent distressing memories
- Nightmares related to the trauma
- Emotional or physical distress when reminded of the event
-
Avoidance Symptoms
- Avoiding people, places, or conversations that trigger memories
- Suppressing thoughts about the traumatic experience
-
Negative Changes in Thoughts and Mood
- Persistent guilt or shame
- Emotional numbness
- Loss of interest in activities
- Feelings of hopelessness
- Difficulty maintaining relationships
-
Changes in Arousal and Reactivity
- Irritability or anger outbursts
- Difficulty sleeping
- Being easily startled
- Hypervigilance
- Risky or self-destructive behavior
When I look at these symptoms together, I see how profoundly PTSD can affect mental health and wellbeing. It touches every aspect of life—sleep, relationships, work, and self-perception.
Who Is at Risk?
PTSD does not discriminate. However, certain factors may increase risk:
- Experiencing intense or prolonged trauma
- Having a history of childhood adversity
- Lacking social support
- Existing mental health conditions
- Family history of psychological disorders
- Ongoing stress after the traumatic event
One important lesson I’ve learned is that resilience is not about avoiding trauma. It’s about having the right support systems and coping mechanisms in place.
PTSD in Children and Adolescents
Children process trauma differently from adults. In young children, PTSD may show up as:
- Regressive behaviors such as bedwetting
- Clinginess
- Play that reenacts traumatic events
- Unexplained fears
In adolescents, it may look like:
- Aggressive behavior
- Academic decline
- Risk-taking behaviors
- Depression or social withdrawal
Promoting mental health awareness in families and schools is critical. Early intervention can prevent long-term psychological health challenges.
Diagnosis of PTSD
PTSD is diagnosed by a qualified mental health professional. Diagnosis typically involves:
- A detailed clinical interview
- Discussion of symptoms and duration
- Evaluation of how symptoms impact daily functioning
For a formal diagnosis:
- Symptoms must last longer than one month.
- Symptoms must cause significant distress or impairment.
- Other medical conditions or substance use must be ruled out.
Seeking professional help is often the hardest step. I’ve seen how stigma around mental health can delay treatment. But early intervention improves outcomes significantly.
Treatment Options for PTSD
Recovery from PTSD is possible. I’ve learned that treatment works best when tailored to the individual. Common treatment approaches include:
-
Psychotherapy
- Cognitive Behavioral Therapy (CBT)
- Trauma-focused CBT
- Exposure therapy
- Eye Movement Desensitization and Reprocessing (EMDR)
- Cognitive Processing Therapy
Therapy helps individuals process trauma safely, reframe negative beliefs, and reduce emotional intensity associated with memories.
-
Medication
- Selective serotonin reuptake inhibitors (SSRIs)
- Anti-anxiety medications
- Sleep aids when necessary
Medication can support mental stability by reducing anxiety, depression, and sleep disturbances.
-
Support Groups
- Peer support groups
- Community mental health programs
- Online support communities
Connecting with others who share similar experiences can reduce feelings of isolation.
Self-Care Strategies to Support Mental Health and Wellbeing
While professional treatment is essential, I’ve seen how lifestyle changes can complement therapy.
- Establishing a consistent sleep routine
- Practicing mindfulness or meditation
- Engaging in regular physical activity
- Maintaining a balanced diet
- Limiting alcohol and substance use
- Building a reliable support network
- Journaling emotions and triggers
- Setting small, achievable goals
These steps may seem simple, but they can significantly strengthen psychological health over time.
The Importance of Mental Health Awareness
One of the biggest barriers to healing is stigma. Mental health awareness helps:
- Normalize conversations about trauma
- Encourage early diagnosis
- Reduce shame and isolation
- Promote empathy and understanding
- Improve access to care
When we talk openly about PTSD, we help others recognize that seeking help is a sign of strength, not weakness.
Long-Term Outlook and Recovery
PTSD is not always a lifelong condition. Many people recover with appropriate treatment and support. Recovery often involves:
- Learning coping mechanisms
- Rebuilding trust in oneself and others
- Strengthening emotional regulation
- Restoring a sense of safety
For some individuals, symptoms may reduce significantly. For others, management becomes part of ongoing mental health care.
I have come to believe that healing from trauma is not about erasing memories. It is about regaining control over how those memories influence the present.
When to Seek Immediate Help
Immediate professional support is crucial if someone experiences:
- Suicidal thoughts
- Self-harm behaviors
- Severe panic attacks
- Substance misuse
- Inability to function daily
Emergency services and crisis helplines should be contacted without delay in such cases.
Supporting Someone With PTSD
If someone close to me were living with PTSD, I would:
- Listen without judgment
- Avoid minimizing their experience
- Encourage professional help
- Learn about the condition
- Be patient with emotional reactions
- Respect their boundaries
Support can make a meaningful difference in someone’s journey toward mental stability.
Conclusion
Post-traumatic stress disorder is a complex but treatable mental health condition. It affects how individuals think, feel, and interact with the world around them. Through increased mental health awareness, early intervention, and compassionate support, recovery becomes possible.
I have learned that trauma does not define a person. With the right resources, therapy, and self-care practices, individuals can rebuild psychological health and strengthen mental health and wellbeing.
Understanding PTSD is not just about clinical definitions. It is about empathy, education, and commitment to supporting those navigating the invisible wounds of trauma.
Healing may take time, but it is absolutely achievable.