Understanding Chronic Venous Insufficiency From a Personal Health Perspective
When I first started learning about circulation problems, I assumed vein-related issues were mostly cosmetic. I thought varicose veins were just visible surface concerns. Over time, I realized that chronic venous insufficiency is far more than a cosmetic condition. It is a progressive circulatory disorder that can significantly affect comfort, mobility, and overall quality of life.
Chronic venous insufficiency happens when the veins in the legs struggle to send blood back to the heart efficiently. Instead of flowing upward smoothly, blood leaks backward and collects in the lower limbs. This backward flow is often referred to as venous incompetence, and the resulting buildup of blood is known as venous pooling.
Understanding how this condition develops, recognizing symptoms early, and seeking appropriate care can make a substantial difference. In this article, I will walk through causes, symptoms, diagnosis, risk factors, cvi treatment options, and prevention strategies in a practical, easy-to-understand way.
-
What Is Chronic Venous Insufficiency?
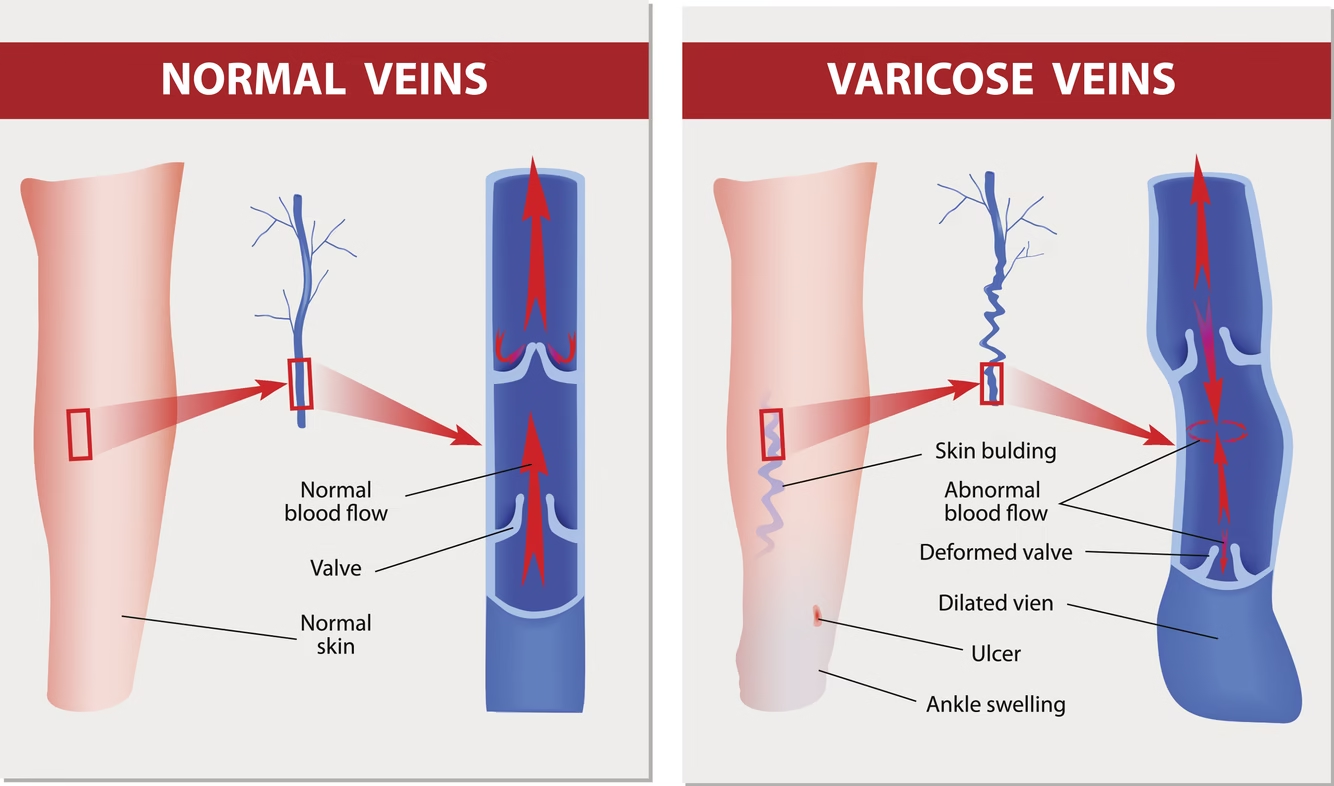
Chronic venous insufficiency, sometimes called cvi disease, is a long-term condition affecting the veins, primarily in the legs. In a healthy circulatory system:
- Veins carry blood from the body back to the heart.
- One-way valves inside veins prevent blood from flowing backward.
- Calf muscles help pump blood upward against gravity.
When these valves become weak or damaged, venous dysfunction develops. Instead of moving upward, blood flows backward and collects in the lower legs. Over time, this increases pressure inside the veins and leads to swelling, discomfort, and skin changes.
CVI legs often appear swollen, heavy, or discolored. In advanced cases, open sores called venous ulcers may develop.
-
How the Veins Normally Work
To truly understand venous incompetence, I had to first understand normal circulation.
- The heart pumps oxygen-rich blood through arteries.
- Oxygen-depleted blood returns through veins.
- Leg veins must work against gravity.
- One-way valves prevent backward flow.
When I visualize it, I imagine a system of locks in a canal. If one lock fails, water moves in the wrong direction. In the same way, faulty valves allow venous pooling in the lower extremities.
Over time, this persistent pressure damages the vein walls and surrounding tissues.
-
Causes of Chronic Venous Insufficiency
There are several causes that contribute to chronic venous insufficiency. In many cases, it develops gradually over years.
-
Damaged or Weak Vein Valves
- Age-related degeneration
- Genetic predisposition
- Long-standing varicose veins
-
Deep Vein Thrombosis
- Blood clots can damage valves permanently
- Post-thrombotic syndrome may develop
-
Prolonged Pressure in Leg Veins
- Standing for long periods
- Sitting without movement
- Obesity increasing venous pressure
When I look at these causes, I see how lifestyle and biology intersect. Some factors are unavoidable, but many are modifiable.
-
Symptoms of CVI Legs
Symptoms often start subtly and worsen over time. Recognizing early signs is crucial.
Early Symptoms
- Leg heaviness
- Aching after long periods of standing
- Mild swelling around ankles
- Visible varicose veins
- Itching or tingling
Progressive Symptoms
- Persistent swelling
- Skin discoloration
- Thickened skin
- Hardening of tissues
- Cramping
Advanced Symptoms
- Venous ulcers near ankles
- Open wounds that heal slowly
- Recurrent infections
The most common pattern I notice is worsening discomfort by the end of the day. Elevating the legs often brings temporary relief.
-
Risk Factors
Several risk factors increase the likelihood of developing chronic venous insufficiency.
-
Age
- Risk increases after 50
- Vein elasticity decreases
-
Gender
- More common in women
- Hormonal influences play a role
-
Pregnancy
- Increased blood volume
- Pressure on pelvic veins
-
Obesity
- Increased abdominal pressure
- Greater strain on leg veins
- Poor calf muscle pumping
- Increased venous pooling
-
Family History
- Genetic weakness of vein walls
- Higher likelihood of venous dysfunction
When I reflect on these factors, I see how prevention strategies can be built around modifiable risks.
-
Diagnosis and Tests
If symptoms suggest cvi disease, a healthcare provider will perform specific evaluations.
-
Physical Examination
- Checking swelling
- Inspecting skin changes
- Assessing varicose veins
-
Duplex Ultrasound
- Measures blood flow
- Detects valve dysfunction
- Identifies clots
This is the most common and non-invasive diagnostic tool.
-
Venography
- Contrast dye imaging
- Used in complex cases
-
Ankle-Brachial Index
- Compares blood pressure in ankle and arm
- Rules out arterial disease
Accurate diagnosis is essential before starting cvi treatment, especially to rule out other circulatory problems.
-
CVI Treatment Options
Treatment depends on severity. I’ve learned that early intervention can prevent complications.
-
Lifestyle Modifications
- Regular walking
- Leg elevation
- Weight management
- Avoiding prolonged standing
-
Compression Therapy
- Compression stockings improve blood flow
- Reduce swelling
- Decrease venous pooling
Compression is often the first-line approach for managing cvi legs.
-
Medications
- Pain relievers
- Topical creams for skin irritation
- Antibiotics for infected ulcers
Medication supports symptom control but does not fix valve damage.
-
Minimally Invasive Procedures
- Endovenous laser therapy
- Radiofrequency ablation
- Sclerotherapy
These procedures close damaged veins and redirect blood flow.
-
Surgical Options
- Vein stripping
- Valve repair
- Vein bypass in severe cases
Surgery is usually reserved for advanced venous dysfunction.
-
Complications of Untreated CVI
Ignoring chronic venous insufficiency can lead to serious issues.
- Chronic leg pain
- Severe swelling
- Venous ulcers
- Skin infections
- Reduced mobility
Venous ulcers, in particular, can significantly impact quality of life and require long-term care.
-
Prevention Strategies
Although not all cases are preventable, I believe consistent habits make a major difference.
-
Maintain Healthy Weight
- Reduces pressure on leg veins
- Improves overall circulation
-
Stay Physically Active
- Walking strengthens calf muscles
- Enhances venous return
-
Avoid Prolonged Sitting or Standing
- Take breaks every hour
- Stretch regularly
-
Elevate Legs
- Elevate above heart level
- Do this several times daily
-
Wear Compression Stockings if Recommended
- Especially during travel
- If at high risk
-
Avoid Tight Clothing Around Waist and Legs
- Prevents restricted blood flow
Prevention often involves small, consistent actions rather than drastic changes.
-
Living With Chronic Venous Insufficiency
Managing cvi disease requires long-term commitment.
- Monitoring symptoms
- Wearing compression regularly
- Following medical advice
- Protecting skin integrity
I see chronic venous insufficiency as a manageable condition when addressed early. Delayed care often leads to avoidable complications.
-
When to Seek Medical Attention
Immediate evaluation is necessary if:
- Sudden swelling in one leg
- Severe pain
- Warmth and redness
- Non-healing wounds
- Signs of infection
Prompt diagnosis ensures safe and effective treatment planning.
Conclusion
Chronic venous insufficiency is more than tired legs. It is a progressive circulatory condition involving venous incompetence and venous pooling that can significantly impact daily life. From mild swelling to serious ulcers, the spectrum of symptoms varies widely.
Through early diagnosis, appropriate cvi treatment, lifestyle adjustments, and preventive measures, long-term complications can often be avoided. Understanding venous dysfunction empowers individuals to take proactive steps toward better vascular health.
When I look at this condition now, I no longer see it as just a vein issue. I see it as a reminder of how important circulation is to overall health and how small daily habits can influence long-term outcomes.