Crohn’s disease is a chronic inflammatory bowel disorder that affects millions of people worldwide. It is one of the main conditions under the category of inflammatory bowel disease (IBD) and can cause persistent inflammation in any part of the digestive tract, from the mouth to the anus. However, it most commonly affects the small intestine and the beginning of the large intestine. Over time, inflammation can penetrate deep into the intestinal layers, leading to pain, digestive complications, and serious health challenges if left untreated.
Although there is currently no cure, effective Crohn’s disease treatment options are available that help manage symptoms, reduce flare-ups, and improve long-term quality of life. Early diagnosis, medical supervision, and lifestyle adjustments play a significant role in controlling this condition.
This comprehensive guide explains the causes, symptoms, risk factors, diagnosis methods, prevention strategies, and treatment options for Crohn’s disease.
What Is Crohn’s Disease?
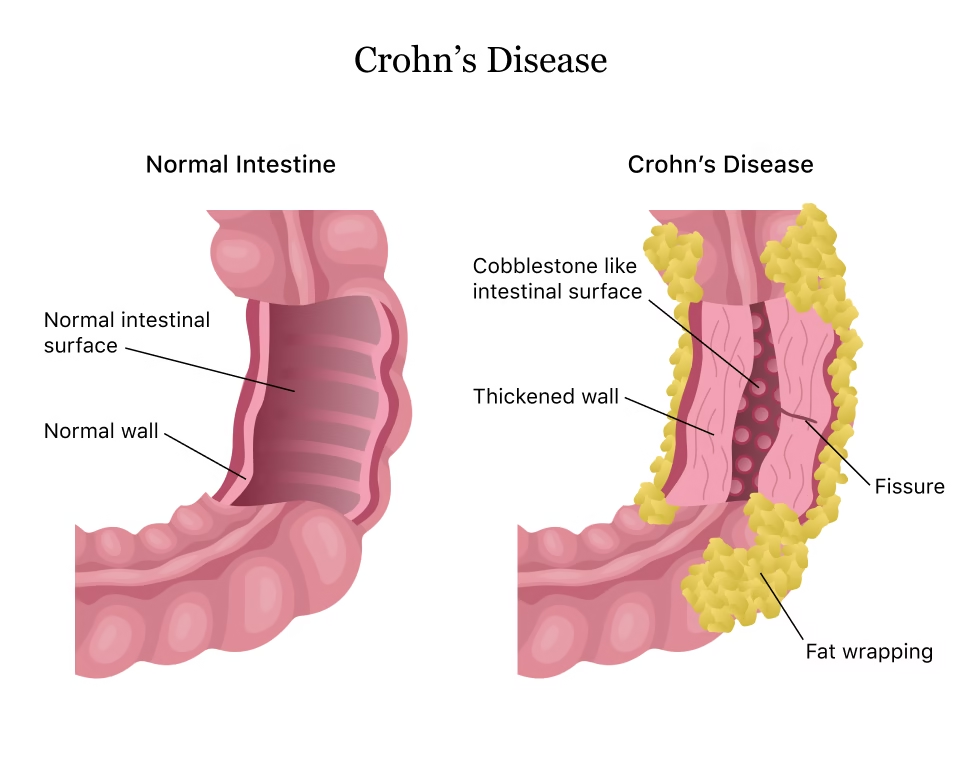
Crohn’s disease is a chronic autoimmune inflammatory disorder of the digestive tract. The exact cause remains unclear, but research suggests that the immune system mistakenly attacks healthy cells in the digestive system, leading to persistent inflammation. Unlike many digestive disorders that affect only surface tissue, Crohn’s inflammation can spread deep through intestinal walls and cause permanent structural damage.
Crohn’s is closely related to ulcerative colitis, another type of IBD. These conditions are often grouped together as colitis and Crohn’s disease, but they differ in how and where they affect the gastrointestinal tract. Ulcerative colitis impacts only the colon and rectum, while Crohn’s can occur anywhere throughout the GI tract.
Crohn’s disease is lifelong, and symptoms come in cycles, with periods of remission and flare-ups. Because it affects nutrient absorption, digestion, and bowel function, it can significantly impact daily life.
Types of Crohn’s Disease
Crohn’s may present differently depending on the affected area. The most common forms include:
-
Ileocolitis
Affects the small intestine (ileum) and the beginning of the colon. Symptoms often include diarrhea, cramping, and significant weight loss.
-
Small Bowel Crohn’s Disease
Occurs primarily in the small intestine, leading to severe malabsorption and nutrient deficiencies.
-
Gastroduodenal Crohn’s
Affects the stomach and upper small intestine, causing nausea, vomiting, and poor appetite.
-
Colitis (Crohn’s Colitis)
Affects the colon only and can resemble ulcerative colitis, leading to bloody stools and frequent bowel movements.
-
Perianal Crohn’s Disease
Causes fissures, abscesses, and fistulas around the anal region.
Understanding the type helps determine appropriate IBD therapy and treatment planning.
Crohn’s Disease Causes
Although the exact cause remains unknown, several factors are believed to contribute:
-
Immune System Dysfunction
The immune system reacts abnormally to harmless bacteria or food, triggering chronic inflammation in the digestive tract.
-
Genetics
People with a family history of Crohn’s have a higher likelihood of developing it.
-
Gut Microbiome Imbalance
An unhealthy gut microbiome may increase intestinal inflammation.
-
Environmental Triggers
Factors such as pollution, chemicals, or infections may initiate inflammatory responses.
-
Lifestyle Factors
Smoking is strongly associated with worsening and more severe Crohn’s disease.
Crohn’s Disease Symptoms
Symptoms vary depending on the location and severity of inflammation. Common signs include:
- Chronic abdominal pain or cramps
- Persistent diarrhea, sometimes with blood
- Sudden weight loss or reduced appetite
- Fatigue and weakness
- Fever during flare-ups
- Bloating and discomfort related to Crohn’s disease stomach
- Vomiting or nausea
- Nutrient deficiency symptoms such as anemia
In advanced cases:
- Fistulas (abnormal tunnels in tissue)
- Bowel obstruction
- Deep ulcers
- Rectal bleeding
Some patients also experience symptoms beyond the digestive system, including:
- Joint pain
- Skin rashes
- Eye inflammation
- Liver complications
Because these symptoms overlap with several gastrointestinal disorders, proper testing is essential for accurate diagnosis.
Risk Factors for Crohn’s Disease
Various factors increase the likelihood of developing or worsening Crohn’s disease:
- Family history
- Age (most common under 35, but can occur at any age)
- Smoking
- High-fat, processed diet
- Living in developed or urban environments
- Autoimmune disorders
- History of gastrointestinal infections
- Ethnicity, including higher incidence in European descent, though now rising globally
Complications of Chronic Crohn’s Disease
If untreated, Crohn’s can cause serious long-term complications such as:
- Intestinal blockage or narrowing
- Malnutrition
- Severe dehydration
- Fistulas or abscesses
- Colon cancer risk increase
- Bone density loss due to nutritional deficiencies
- Poor growth in children
This is why early assessment, lifestyle modification, and consistent medical care are crucial.
Diagnosis and Tests for Crohn’s Disease
There is no single test to confirm Crohn’s, so doctors use a combination of methods.
Diagnostic Tests Include:
- Blood tests
- Detect anemia, inflammation markers, or infection
- Stool tests
- Check for infection or inflammatory biomarkers
- Colonoscopy
- Allows visual inspection and biopsy collection
- Endoscopy
- Used to examine the upper digestive tract
- CT or MRI scans
- Assess inflammation depth and identify obstructions or fistulas
- Capsule endoscopy
- Patient swallows a tiny camera to view inaccessible areas of intestines
- Celiac and food allergy testing
- Used to rule out similar disorders
Doctors sometimes request a Crohn’s disease blood test to check for antibodies associated with autoimmune disorders.
Crohn’s Disease Treatment Options
Treatment varies based on disease severity, flare frequency, and affected digestive areas. The goal is to manage inflammation, reduce symptoms, prevent complications, and maintain remission.
-
Medications
Common categories include:
- Anti-inflammatory drugs
- Immune system suppressors
- Corticosteroids for severe flare-ups
- Antibiotics for infections and fistulas
- Biologic therapies that target specific immune pathways
- Pain relievers for Crohn’s disease pain, used with caution under medical supervision
Biologic medications have significantly improved outcomes for many people living with chronic Crohn’s disease.
-
IBD Therapy
Often includes a combination of medications and supportive interventions such as nutrition therapy, vitamin supplementation, and stress management.
-
Diet and Nutrition
Certain foods can trigger inflammation or worsen digestion, especially during flare-ups. A structured Crohn’s disease diet helps minimize discomfort.
Helpful dietary strategies include:
- Smaller, more frequent meals
- Low-fiber foods during flare-ups
- Avoiding alcohol, caffeine, and spicy foods
- Reducing dairy if lactose-intolerant
- Staying hydrated
- Working with a nutritionist for personalized planning
-
Lifestyle Modifications
- Quitting smoking
- Reducing stress through yoga, counseling, or meditation
- Moderate exercise
- Adequate sleep
-
Surgery
Required when complications such as intestinal blockage or severe bleeding occur. Surgery may involve removing damaged portions of bowel or repairing fistulas.
While surgery does not cure Crohn’s, it can provide long periods of remission.
Crohn’s Disease Prevention
There is no guaranteed prevention strategy, but healthy habits can significantly reduce flare-ups and slow disease progression.
Prevention tips include:
- Avoid smoking or exposure to smoking environments
- Maintain a nutrient-rich, whole-food diet
- Manage stress proactively
- Follow prescribed medication consistently
- Avoid trigger foods identified through tracking
- Schedule regular medical checkups
- Build a balanced lifestyle supporting gut health
Living with Crohn’s Disease
Crohn’s is a lifelong condition, and managing it successfully requires long-term commitment and support. Many people with Crohn’s live full, active lives by combining Crohn’s disease treatment, nutrition support, mental wellness strategies, and preventive care.
Support groups, both online and in-person, can help individuals emotionally and socially. Patients should work closely with healthcare providers to monitor symptoms and adjust treatment plans as needed.
Final Thoughts
Crohn’s disease is a complex and chronic inflammatory condition that affects digestion, immune function, and overall quality of life. While it cannot be cured, early diagnosis, consistent medical care, supportive therapy, and lifestyle choices can significantly reduce symptom severity and prevent complications. Understanding triggers, recognizing symptoms early, and seeking expert guidance helps individuals maintain stability, reduce flare-ups, and live healthier lives.