When we talk about childbirth, most conversations focus on contractions, dilation, and the final push. Rarely do we talk about what happens if the baby’s shoulders get stuck after the head has been delivered. Yet for a small percentage of births, this is exactly what happens.
The term for it is shoulder dystocia.
It is one of those obstetric emergencies that can sound frightening when you first hear about it. But like many complications in childbirth, what makes the difference is preparation, awareness, and prompt action. Over the years, I’ve noticed that many expectant parents are unaware of what shoulder dystocia maneuvers involve or what factors can increase the risk.
Understanding this topic does not mean expecting the worst. It means being informed.
Let’s walk through it calmly and clearly.
What Is Shoulder Dystocia?
Shoulder dystocia occurs when, after the baby’s head is delivered, one or both shoulders become lodged behind the mother’s pelvic bone. The head is out, but the body cannot follow easily.
This situation requires immediate attention because prolonged delay in delivering the shoulders can reduce oxygen supply to the baby.
It is important to understand that shoulder dystocia is unpredictable in many cases. It can happen even in pregnancies with no obvious risk factors. However, certain conditions increase the likelihood.
Why It Happens
During a typical vaginal birth, the baby’s shoulders rotate slightly to pass through the pelvis. In shoulder dystocia, that rotation does not occur smoothly.
The most common scenario is when the baby’s anterior shoulder becomes stuck behind the mother’s pubic bone. Less commonly, the posterior shoulder can become trapped.
The causes are usually related to:
- Baby size relative to the pelvis
- Maternal conditions affecting fetal growth
- Labor progression patterns
But again, it is not always predictable.
Risk Factors for Shoulder Dystocia
Although shoulder dystocia can occur without warning, research has identified factors that increase risk.
The most significant risk factors include:
- Fetal macrosomia (larger-than-average baby)
- Maternal diabetes (gestational or preexisting)
- Previous history of shoulder dystocia
- Excessive maternal weight gain
- Prolonged second stage of labor
- Operative vaginal delivery (forceps or vacuum use)
- Post-term pregnancy
Babies of mothers with diabetes are at higher risk because they may develop broader shoulders relative to head size.
However, it is equally important to emphasize that many women with these risk factors deliver without complications. Risk does not equal certainty.
What Happens During Shoulder Dystocia?
When shoulder dystocia occurs, the healthcare team moves quickly. There is no time for panic.
You may hear the team call out the diagnosis. From that moment, coordinated action begins.
The goal is simple: free the shoulder safely and deliver the baby as quickly as possible while minimizing injury.
This is where shoulder dystocia maneuvers come into play.
First-Line Shoulder Dystocia Maneuvers
The first approach is usually non-invasive and focuses on repositioning the mother to widen the pelvic outlet.
McRoberts Maneuver
The McRoberts maneuver is often the first and most effective intervention.
In this maneuver:
- The mother’s legs are sharply flexed back toward her abdomen.
- This position flattens the lower spine.
- The angle of the pelvis changes, creating more space for the baby’s shoulder.
The McRoberts maneuver alone resolves a large percentage of shoulder dystocia cases. It is simple, quick, and does not require instruments.
Often, gentle downward traction is applied simultaneously to help guide the shoulder.
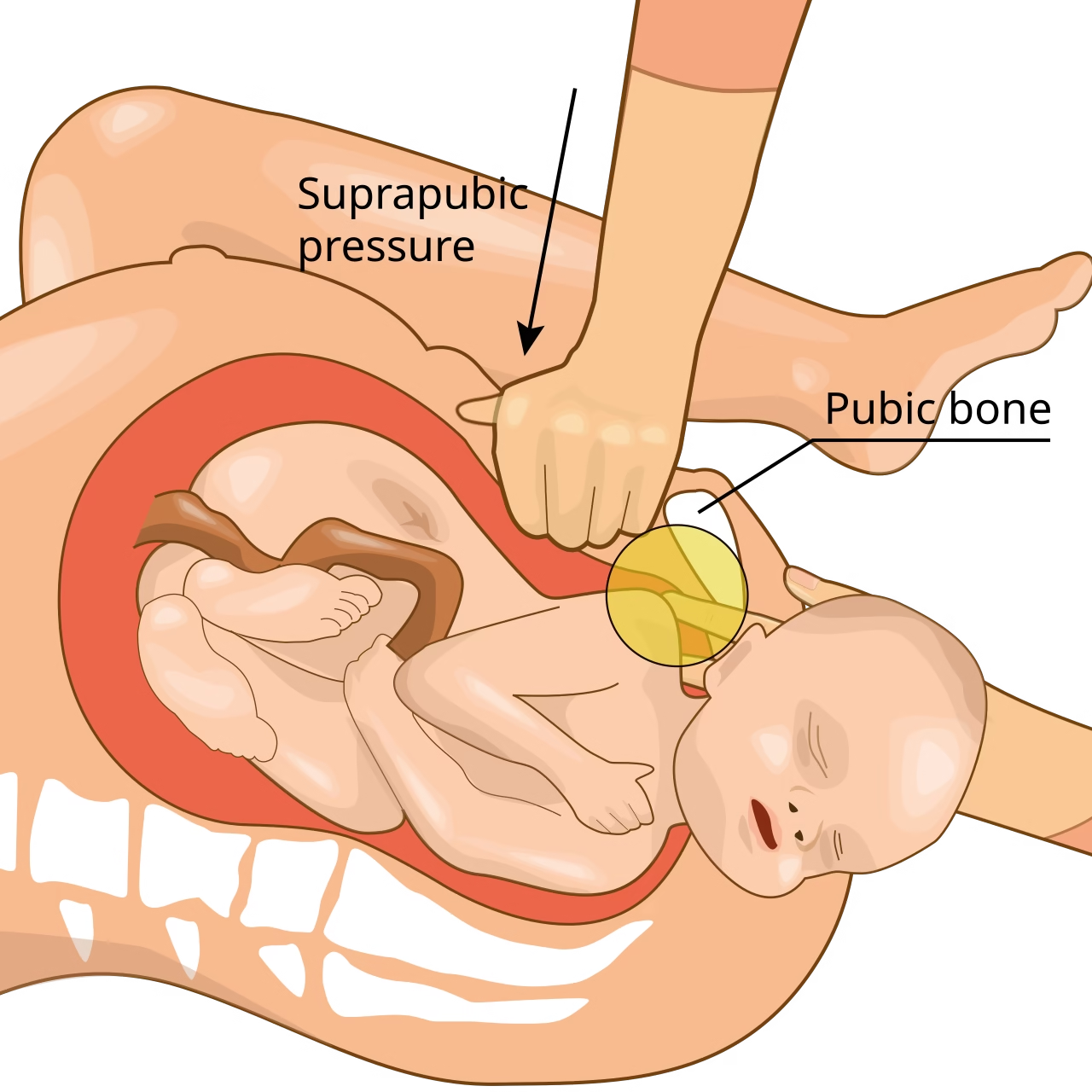
Suprapubic Pressure
If McRoberts alone is not sufficient, the provider may apply suprapubic pressure.
This involves:
- Applying firm pressure just above the pubic bone.
- Attempting to push the baby’s shoulder into a more favorable position.
- Helping rotate the shoulder under the pubic bone.
It is important to note that fundal pressure (pushing on the top of the uterus) is avoided because it can worsen the impaction.
Secondary Shoulder Dystocia Maneuvers
If initial steps are unsuccessful, additional techniques are used.
Gaskin Maneuver for Shoulder Dystocia
The Gaskin maneuver involves repositioning the mother onto her hands and knees.
This all-fours position can:
- Change pelvic dimensions.
- Encourage natural rotation of the baby.
- Relieve pressure on the impacted shoulder.
The Gaskin maneuver for shoulder dystocia is particularly useful in settings where mobility is possible and the mother is not restricted by anesthesia.
Internal Rotational Maneuvers
These involve the provider inserting a hand into the birth canal to rotate the baby’s shoulders manually.
The aim is to:
- Rotate the shoulders into a diagonal position.
- Free the impacted shoulder.
- Reduce shoulder width during passage.
These techniques require skill and experience.
When Is Shoulder Dystocia Surgery Needed?
In rare and extreme cases where standard shoulder dystocia treatment does not succeed, more advanced interventions may be necessary.
These may include:
- Intentional clavicle fracture to reduce shoulder width.
- Zavanelli maneuver (replacing the baby’s head into the birth canal followed by emergency cesarean section).
- Emergency cesarean delivery if feasible.
Shoulder dystocia surgery is rare and considered only when all other measures fail.
It is important to understand that these scenarios are uncommon.
Shoulder Dystocia Treatment After Birth
Once the baby is delivered, immediate evaluation begins.
For the baby, providers assess:
- Breathing and oxygen levels.
- Arm movement and nerve function.
- Signs of fracture or injury.
Treatment for shoulder dystocia in newborns may include:
- Observation for mild nerve injury.
- Physical therapy if needed.
- Monitoring for clavicle fractures.
- Oxygen support if there was temporary distress.
Most babies recover well, particularly when the condition is managed promptly.
For the mother, shoulder dystocia treatment after birth may involve:
- Repair of any perineal tears.
- Monitoring for postpartum hemorrhage.
- Pain management.
- Emotional support and counseling.
The emotional impact should not be underestimated. Even when outcomes are positive, the experience can feel frightening.
Potential Complications
Although many cases resolve without lasting effects, possible complications can include:
For the baby:
- Brachial plexus injury (temporary or permanent nerve damage affecting arm movement).
- Clavicle fracture.
- Oxygen deprivation if delivery is delayed.
For the mother:
- Severe perineal tears.
- Postpartum bleeding.
- Uterine rupture (rare).
Again, with trained providers and rapid response, serious outcomes are uncommon.
Can Shoulder Dystocia Be Prevented?
Prevention is complex because prediction is imperfect.
However, steps that may reduce risk include:
- Good blood sugar control in diabetic pregnancies.
- Monitoring fetal growth.
- Discussing delivery options if the baby is significantly large.
- Considering planned cesarean delivery in very high-risk cases.
Decision-making should always be individualized.
Elective cesarean section is not routinely recommended for all large babies because shoulder dystocia remains relatively rare overall.
The Importance of Prepared Teams
One reassuring aspect is that obstetric teams train regularly for shoulder dystocia emergencies.
Simulation drills allow providers to practice shoulder dystocia maneuvers in controlled settings so that responses become automatic during real situations.
This preparation significantly improves outcomes.
For expectant parents, knowing that your provider is trained in emergency maneuvers can offer peace of mind.
Emotional Recovery Matters Too
While medical management is critical, emotional processing is equally important.
Some mothers report feeling:
- Shock.
- Fear.
- Guilt.
- Anxiety in subsequent pregnancies.
It is important to remember that shoulder dystocia is not caused by anything a mother did wrong.
If you experience it, discussing it with your healthcare provider afterward can help clarify what happened and what future risks may look like.
Looking Ahead After Shoulder Dystocia
If you have experienced shoulder dystocia in a previous delivery, your provider will assess recurrence risk carefully.
Factors considered include:
- Baby’s birth weight.
- Severity of prior complication.
- Presence of diabetes.
- Overall maternal health.
Some women may be offered a planned cesarean in future pregnancies depending on circumstances.
Each case is unique.
Final Thoughts
Shoulder dystocia is one of those childbirth complications that sounds alarming because of its urgency. But it is also one of the most rehearsed and managed obstetric emergencies.
Understanding shoulder dystocia maneuvers such as the McRoberts maneuver and the Gaskin maneuver for shoulder dystocia helps demystify the process.
Yes, certain factors can increase your risk for shoulder dystocia. But risk does not mean inevitability.
The most important takeaway is this:
Prepared providers.
Rapid action.
Calm coordination.
Those are what truly influence outcomes.
If you are pregnant and concerned about risk factors, the best step is an open discussion with your healthcare provider. Knowledge reduces fear, and preparation builds confidence.
Childbirth carries uncertainties, but modern obstetrics has developed structured shoulder dystocia treatment protocols precisely to manage those uncertainties safely.
And in most cases, both mother and baby do well.